Thieme旗下重症监护领域的期刊是研究人员、专家和从业人员公认的首选资源。欢迎免费访问本期的精选论文。
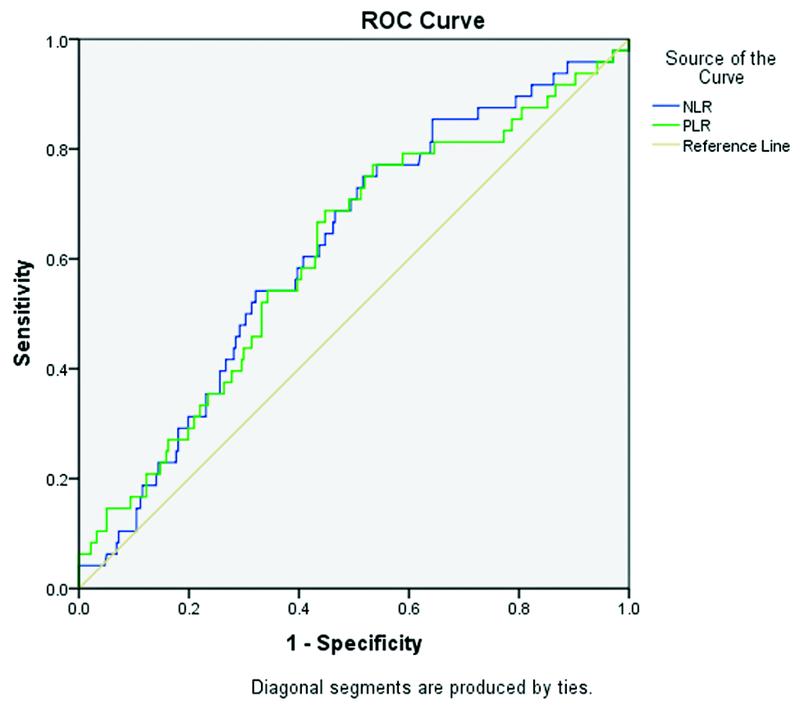
Shenoy & Patil发表在Journal of Pediatric Intensive Care上的研究,旨在确定中性粒细胞淋巴细胞比率 (NLR) 和血小板淋巴细胞比率 (PLR) 预测疾病严重程度的能力和结果,这两个评分系统即儿科后勤器官功能障碍 2 (PELOD-2) 和儿科死亡风险 III (PRISM-III) 。
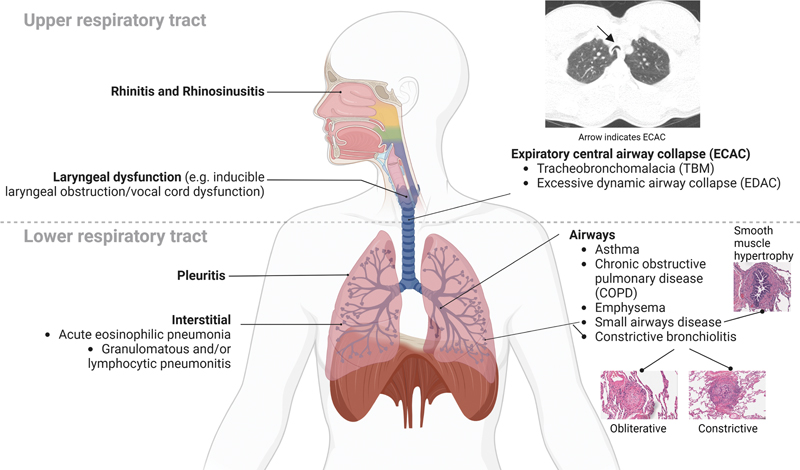
自1990年以来,部署在阿富汗、伊拉克和西南亚(SWA)部分地区的军人和退伍军人面临出现一系列呼吸道症状和部署相关的呼吸道疾病(DRRD)的风险。Krefft & Zell-Baran发表在Seminars in Respiratory and Critical Care Medicine上的评论,旨在总结我们目前对DRRD的理解,并告知肺科医生DRRD筛查、诊断、评估和管理的最新进展。

影响因子2021:3.921
Journal of Pediatric Intensive Care
Sangeetha Shenoy, Shruti Patil
The aim of this study was to determine the ability of neutrophil lymphocyte ratio (NLR) and platelet lymphocyte ratio (PLR) to predict the severity of illness as assessed by two scoring systems, namely, Pediatric Logistic Organ Dysfunction-2 (PELOD-2) and Pediatric Risk of Mortality-III (PRISM-III) and outcome. This was a retrospective cohort study wherein all critically ill children aged 1 month to 18 years admitted in the pediatric intensive care unit from January 2021 to October 2022 were included. Children with chronic systemic diseases and hematological illness were excluded from the study. Demographic details, diagnosis, PRISM-III-24 and PELOD-2 scores at admission, and outcome were retrieved from the hospital case records. NLR and PLR values were compared among high and normal PRISM-III and PELOD-2 groups as well as among survivors and nonsurvivors. A total of 325 patients with critical illness were included with a mean (standard deviation) age of 7(5) years and a male: female ratio of 3:2. The values of NLR were significantly higher among the patients with high PRISM-III (2.2 vs. 1.3, p-value = 0.006) and PELOD-2 (2 vs. 1.4, p-value = 0.015) groups compared with normal. The NLR and PLR were significantly higher among the nonsurvivors compared with the survivors (2.3 vs. 1.4, p-value = 0.013, and 59.4 vs. 27.3, p-value = 0.016 for NLR and PLR, respectively). The area under the receiver operating characteristics curve for NLR and PLR was 0.617 and 0.609, respectively. A high PLR, PRISM-III, and PELOD-2 were the factors found to be independently associated with mortality on multiple logistic regression analysis. Patients with high NLR are associated with more severe illness at admission. NLR and PLR are useful parameters to predict mortality.
Seminars in Respiratory and Critical Care Medicine
Silpa D. Krefft, Lauren M. Zell-Baran
Military personnel and veterans who have deployed to Afghanistan, Iraq, and parts of Southwest Asia (SWA) since 1990 are at risk of developing a host of respiratory symptoms and deployment-related respiratory diseases (DRRDs). This review aims to summarize our current understanding of DRRD and inform pulmonary practitioners of recent updates to DRRD screening, diagnosis, evaluation, and management. The most common respiratory diseases in these patients include asthma, chronic sinonasal disease, laryngeal disease/dysfunction, and distal lung disease. Pulmonary function testing and chest imaging are the most commonly used diagnostic tools, but techniques such as lung clearance index testing via multiple breath washout, forced oscillation testing/impulse oscillometry, and quantitative chest computed tomography (CT) assessment appear promising as noninvasive modalities to aid in lung disease detection in this population. We also summarize guidance on conducting an occupational and deployment exposure history as well as recommendations for testing. Finally, we discuss the Sergeant First Class Heath Robinson Honoring our Promise to Address Comprehensive Toxics Act of 2022 (PACT Act) that includes a list of health conditions that are “presumptively” considered to be related to SWA military deployment toxic exposures, and provide resources for clinicians who evaluate and treat patients with DRRD.